Congenital Hyperinsulinism (CHI) is a rare but serious genetic condition in which the pancreas produces too much insulin, leading to dangerously low blood sugar levels (hypoglycemia). Early diagnosis and treatment are essential to prevent permanent brain damage and ensure a better quality of life.

Congenital Hyperinsulinism (CHI) is a rare genetic disorder of pancreatic β-cells that secrete excess amount of insulin causing severe persistent hypoglycemia (low blood glucose) in new-born babies and children.
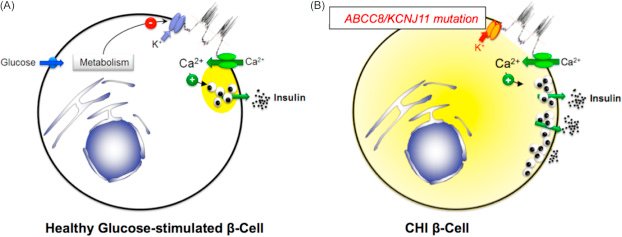
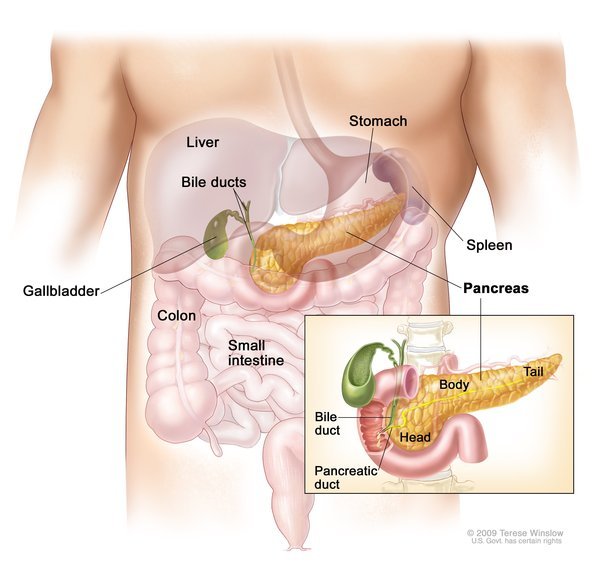
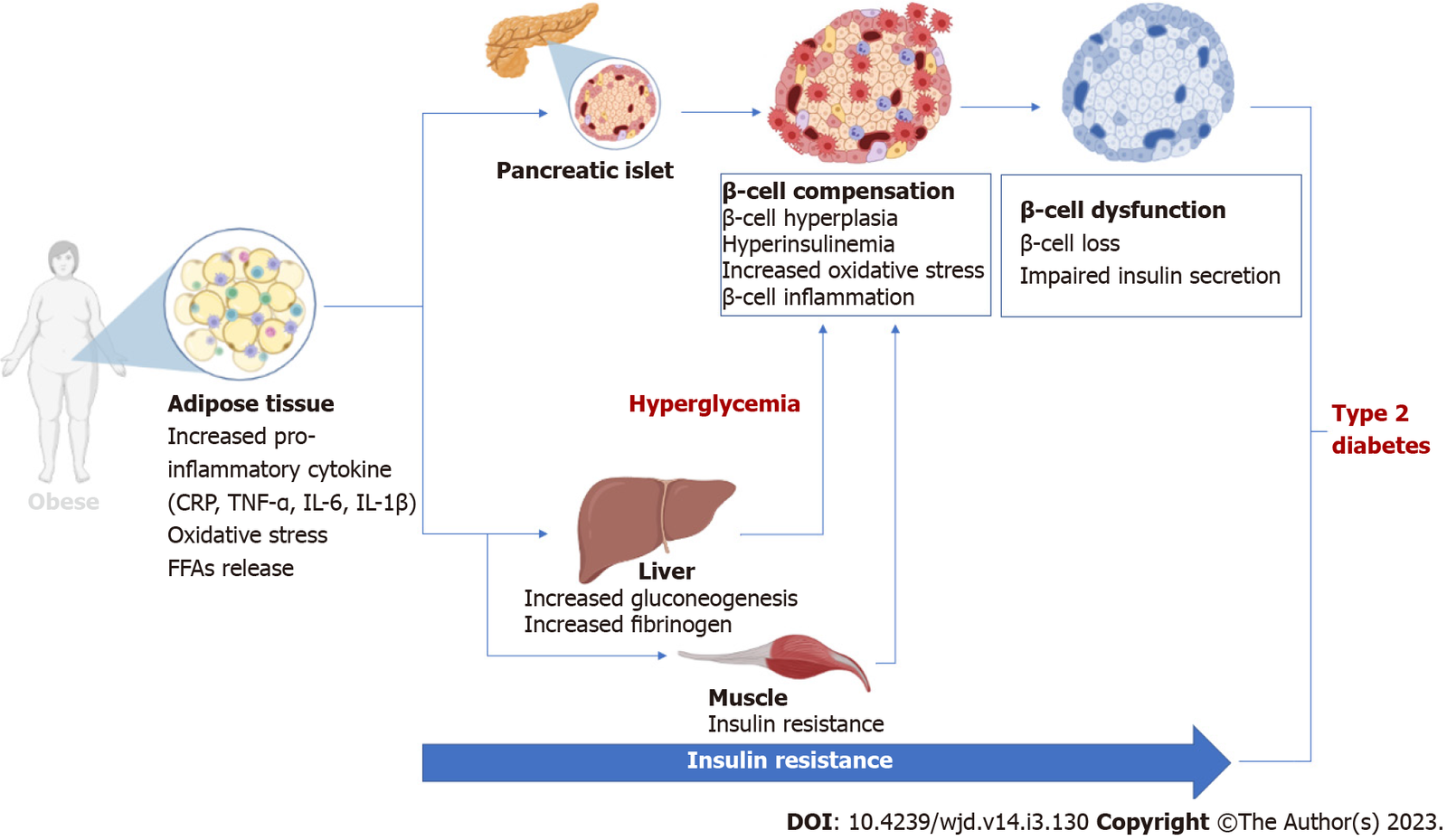
Insulin, a hormone secreted by the β-cells of the islets of Langerhans of pancreas, is chiefly involved in the regulation of carbohydrate (glucose) metabolism. Any increase in blood glucose (sugar) concentration is the most important physiologic factor leading to insulin secretion. Insulin in turn leads to break down of glucose (glycolysis) into energy thereby decreasing glucose concentration in the blood. Additionally, insulin also prevents formation of new glucose (gluconeogenesis) conversion of fat into ketones (ketogenesis), which act alternative fuel for the body in absence of glucose.
Typically, child with hyperinsulinism will have detectable / raised insulin concentrations (hyper-insulinemic) with low ketone bodies (hypoketotic) and free fatty acids (hypo-fatty-acidemic) at the time of low blood glucose concentration (hypoglycemia).
CHI causes repeated episodes of hypoglycemia because of dysregulated insulin secretion during low blood glucose concentrations in newborn babies and children. As a result, insulin suppresses ketone bodies formation and this unavailability of glucose and alternative fuels (ketone bodies) increase the risk of brain damage in these patients.
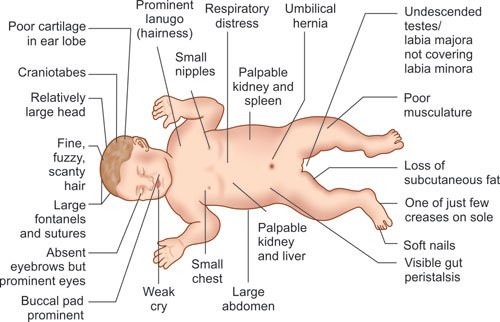
Approximately 60% of the babies with CHI develop hypoglycemia during the first month of life, 30% develop it later in the first year and the remaining even after that.
The sign and symptoms of CHI are due to hypoglycemia and are non-specific during early period making its diagnosis difficult. It is also important to note that babies / children could be asymptomatic (no sign or symptoms) during hypoglycemia and is due to repeated episodes of hypoglycemia. Hence it is important to test blood glucose concentrations.
Common symptoms of hypoglycemia include:
More severe symptoms can occur with long periods of hypoglycemia and can lead to:
At later ages, the symptoms of CHI can be easier to recognize such as:
With early diagnosis and treatment to hypoglycemia, brain damage can be prevented.
There are two primary forms of CHI:
Genetic testing and advanced imaging help distinguish between the two, which is important for determining the right treatment approach.
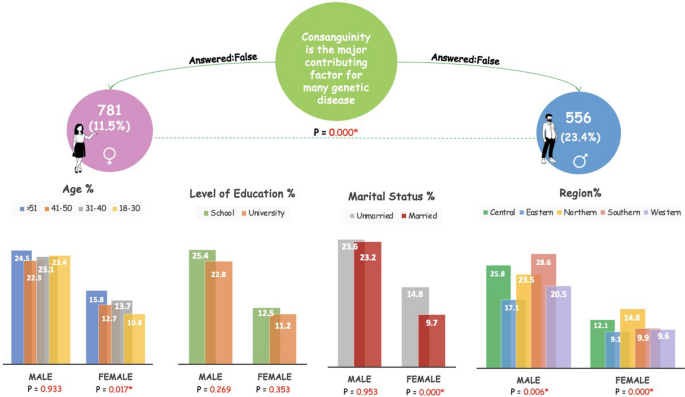
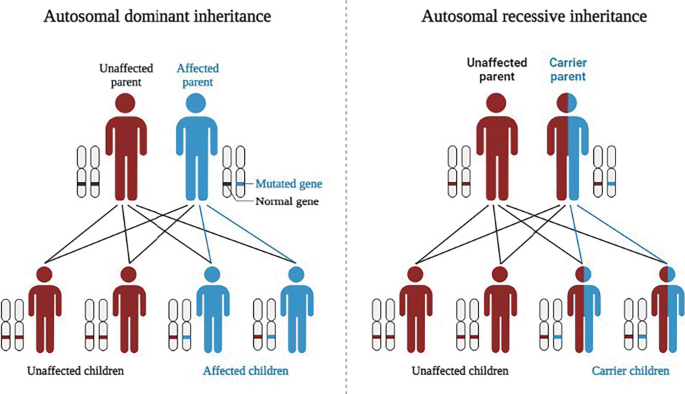
An autosomal recessive pattern means both copies of genes passed on from each parent in the cell has mutations. Whereas in autosomal dominant pattern one copy of the altered gene in passed on from either of the parent.
Congenital Hyperinsulinism is a genetic disorder with different inheritance patters, usually depending on the form of the condition.
Early diagnosis is crucial and includes:
A diagnosis is confirmed when low blood glucose coincides with inappropriately high insulin levels and suppressed ketones and fatty acids.
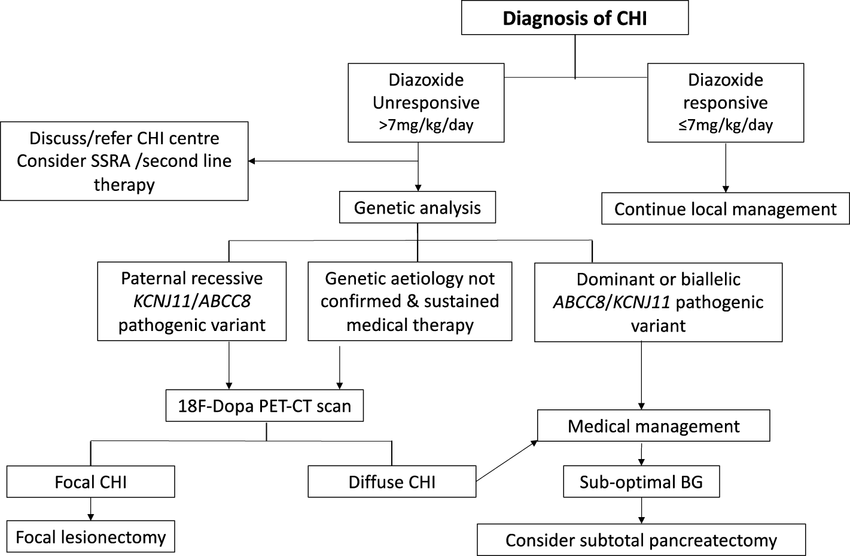
Treatment depends on the type and severity of CHI:
Early and individualized treatment reduces the risk of brain injury and improves long-term outcomes.